Practice Policies & Patient Information
Access To Medical Records
Data subjects have the right to have access to data held on them using a Subject Access Request (SAR) process and withdraw existing consent to access and use of their data by an organisation.
There is no set format for submitting a Subject Access Request. It can be done in writing, in person or over the phone; however to assist the process the Practice recommends that our Subject Access Form is completed (below).
Data will only be released to the subject therefore it is imperative that the subject is identified. Where the Practice has not retained copies of patient’s identity, due to legacy regulation pertaining to identification and retention of records, patient will be asked to verify their identity prior to data being released.
Prior to the release of documents, the Practice has a legal duty to review them and remove any information that identifies third parties or may cause harm or distress to the subject. The Practice has an obligation to provide information requested through a Subject Access Request within 28 days.
Alternatively, if you are already an online user, you can request limited access to your detailed coded records by completing a dedicated form within the online systems.
Compliments & Complaints

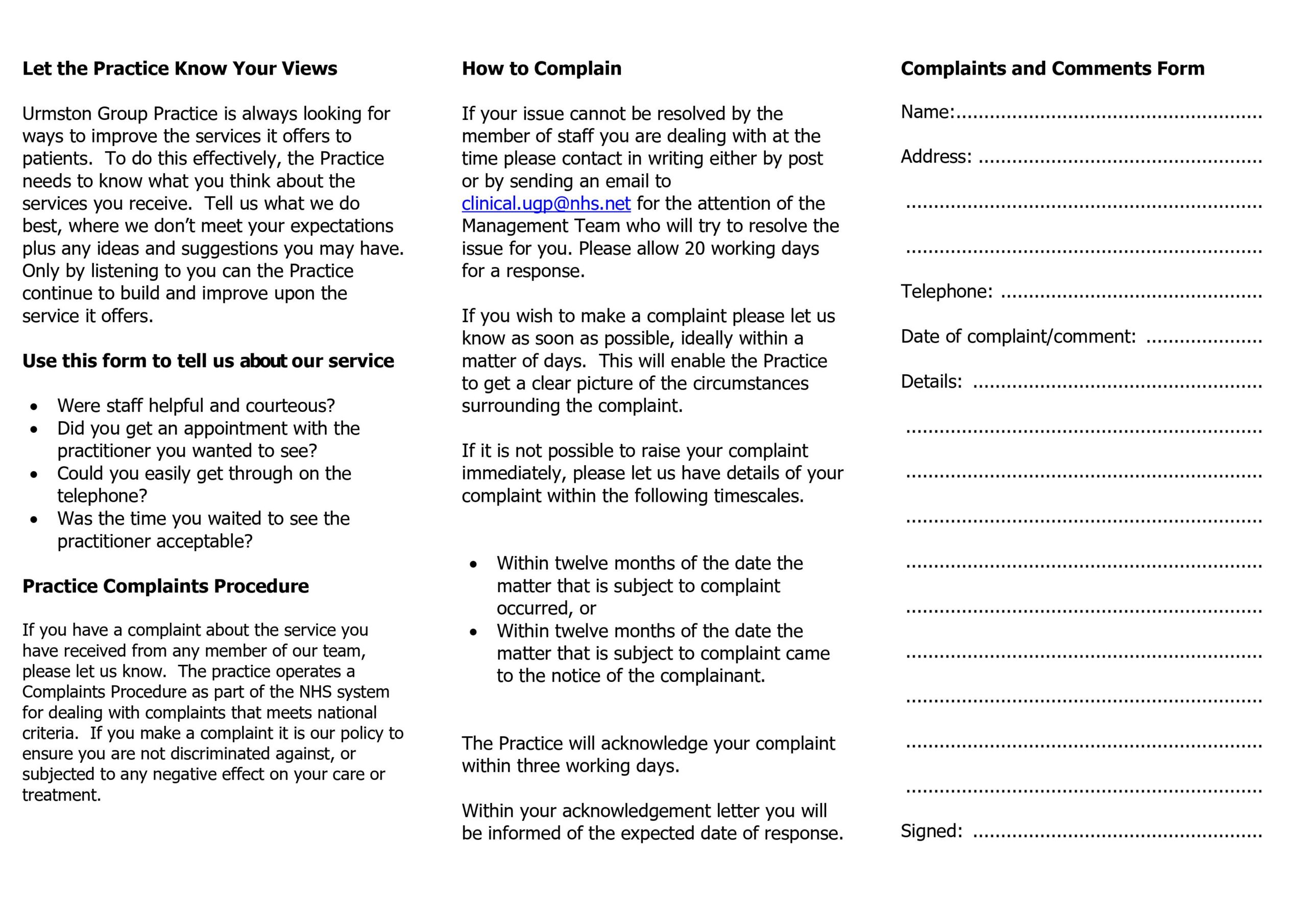
We make every effort to give the best service possible to everyone who attends our practice.
However, we are aware that things can go wrong resulting in a patient feeling that they have a genuine cause for complaint. If this is so, we would wish for the matter to be settled as quickly, and as amicably, as possible.
To pursue a complaint please contact the practice management team who will deal with your concerns appropriately. Further written information is available regarding the complaints procedure from reception.
If you are dissatisfied with the outcome you may refer the matter to The Parliamentary & Health Service Ombudsman for their consideration, find guidance on their website www.ombudsman.org.uk/making-complaint (their leaflet may help).
Infection Control Statement
This practice is committed to the control of infection within the building and in relation to the clinical procedures carried out within it.
The practice will undertake to maintain the premises, equipment, drugs, and procedures to the standards detailed within the Checklist and will undertake to provide facilities and the financial resources to ensure that all reasonable steps are taken to reduce or remove all infection risks.
Wherever possible or practicable the practice will seek to use washable or disposable materials for items such as soft furnishings and consumables, e.g. seating materials, wall coverings including paint, bedding, couch rolls, modesty sheets, bed curtains, floor coverings, towels, etc., and ensure that these are laundered, cleaned or changed frequently to minimise the risk of infection.
We aim to keep our practice clean and tidy and offer a safe environment to our patients and staff and we endeavor to ensure it is kept clean and well always maintained.
All clinicians follow our Infection Control Policy to ensure the care we deliver and the equipment we use is safe.
We take additional measures to ensure we maintain the highest standards:
- Encourage staff and patients to raise any issues or report any incidents relating to cleanliness and infection control. We can discuss these and identify improvements we can make to avoid any future problems.
- Carry out an annual infection control audit to make sure our infection control procedures are working.
- Provide annual staff updates and training on cleanliness and infection control
- Review our policies and procedures to make sure they are adequate and meet national guidance.
- Maintain the premises and equipment to a high standard within the available financial resources and ensure that all reasonable steps are taken to reduce or remove all infection risk.
- Use washable or disposable materials for items such as couch rolls, modesty curtains, floor coverings, towels etc, and ensure that these are laundered, cleaned or changed frequently to minimise the risk of infection.
- Make Alcohol Hand Rub Gel available throughout the building.
Online Access to Medical Records
There are different levels of online access available to patients. Registration for access to medical records can be made in person or online (clinical.ugp@nhs.net) photo ID required.
- Basic: Repeat Prescriptions and Summary Information
- Detailed Coded Record: Appointments, Repeat Prescriptions and Detailed Coded Record Access
Basic Access
If you wish to apply for basic online access to your medical records please contact the surgery for more information or complete the request form below and return to the surgery.
You can also now see new information that is added to your online health record. This information includes notes from your appointment as well as test results and any letters about future appointments. You can see this through the NHS App, website or another health app such as Patient Access.
Basic Access Online Registration Form
Please note that to access your records online you will be requested to provide ID verification to ensure that users have a legitimate right to view the health records.
Detailed Coded Record Access
You will need Basic online access before requesting Detailed Coded Record access.
The practice will not automatically grant access to Detailed Coded Record Access.
Patients wanting access to their Detailed Coded Information must complete and submit a DCR Patient Online Access Application Form which is available below.
We also have a Patient Information Leaflet which provides more detail on this online access service (below), copies are also available from reception.
Information Leaflet – Online Access to Medical Services
What are detailed coded records?
Detailed coded records hold medical information; GPs access this when in an appointment. This includes information about:
- Demographics
- Conditions/diagnoses,
- Medications
- Allergies
- Immunisations
- Results
- Values (like blood pressure)
- Coded information about procedures, referrals and consultations.
- Some administrative information is also coded in the patient record.
Documents attached to the record, like letters, and free text are not always included.
Detailed Coded Record Access Request Form
Proxy Access
Proxy online access is not currently available for patients aged between 12-15 years old unless a clinician decides it is in the child’s best interest.
Patient Confidentiality
The practice complies with data protection and access to medical records legislation. Identifiable information about you will be shared with others in the following circumstances:
- To provide further medical treatment for you e.g. from district nurses and hospital services.
- To help you get other services e.g. from the social work department. This requires your consent.
- When we have a duty to others e.g. in child protection cases anonymised patient information will also be used at local and national level to help the Health Board and Government plan services e.g. for diabetic care.
If you do not wish anonymous information about you to be used in such a way, please let us know.
Reception and administration staff require access to your medical records in order to do their jobs. These members of staff are bound by the same rules of confidentiality as the medical staff.
Freedom of Information
Information about the General Practitioners and the practice required for disclosure under this act can be made available to the public. All requests for such information should be made to the practice manager.
Summary Care Record
The Central NHS Computer System called the Summary Care Record (SCR) is an electronic record which contains information about the medicines you take, allergies you suffer from and any bad reactions to medicines you have had.
Why do I need a Summary Care Record?
Storing information in one place makes it easier for healthcare staff to treat you in an emergency, or when your GP practice is closed.
This information could make a difference to how a doctor decides to care for you, for example which medicines they choose to prescribe for you.
Who can see it?
Only healthcare staff involved in your care can see your Summary Care Record.
How do I know if I have one?
Over half of the population of England now have a Summary Care Record. You can find out whether Summary Care Records have come to your area by asking your GP
Do I have to have one?
No, it is not compulsory. If you choose to opt out of the scheme, then you will need to complete a form and bring it along to the surgery. Click here for the the Opt Out Form.
More Information
For further information visit the NHS Care records website.
GDPR
Patient Information – under the new GDPR (General Data Protection Regulations) from 25 May 2018 there is a new law that determines how your personal data is kept safe and processed and the legal rights you have in relation to your own data.
What do we mean by ‘accessing health records’?
This means that you can see and/or have copies of your health records. these records could be those at the hospital or those held by your GP, dentist, pharmacist or optician. They also include records written by health visitors, district nurse and other community staff as well as the ambulance service. Records include xrays, scan, reports etc.
Why would I want to access my health records?
You may want to know what’s been written in your health records for many reasons. You may be thinking of making a complaint about your healthcare. You do not need to tell anyone the reasons why you want access to your health records
Will I have to pay any charges?
No under the new GDPR (General Data Protection Regulation) there is now no fee providing there is not an unreasonable number of requests received in a short period of time.
Are there any date or time restrictions on health records that I can access?
No. You can request access to any health records that you know exists
How long should it take for my request to be processed?
You should be able to view and/or have copies of your health records within 28 days of your request being made and any necessary fee being paid.
What if I am requesting access to health records of somebody who has died?
Your rights are different. As duty of confidentiality survives a patient’s death then you have to have good reasons for wanting access. This may be because you are:
- the patient’s personal representative
- an executor of their will
- a person granted letters of administration by the probate registry or
- a person with a claim arising out of the patient’s death
- you can only access health records that were made from 1 November 1991. Similar charges apply as above. You can ask for somebody to be present, to provide any necessary explanations of what is written in the health records
Can my request be refused?
Yes. Where the record holder feels that it would cause serious harm to the physical or mental health of you or anyone else then you may be refused access. If you are refused access for this reason then you have the right to be advised about this refusal.
Practice Policy on Prescribing Diazepam
Benzodiazepines (including diazepam, lorazepam, temazepam, clonazepam) are medicines that have been in use since the 1960s for a wide range of conditions, such as alcohol withdrawal, epilepsy, and muscle spasms. They are strongly sedating drugs that have negative effects on memory, coordination, concentration, and reaction times. They are addictive and withdrawal can lead to seizures, hallucinations, agitation, and confusion.
Unfortunately, benzodiazepines have widely become drugs of abuse, and as a result they are controlled in the UK as Class C, Schedule 4 drugs. This means there are restrictions on when and how much can be prescribed under the Controlled Substances Act, and inappropriate use, supply or possession of these medications is illegal in the UK under the Misuse of Drugs Act.
Many people approach their GP practice asking for diazepam to help with fear of flying, or to sleep during a flight. There are several good reasons why prescribing diazepam is not recommended, and as a result we will no longer prescribe diazepam for patients who wish to use this for a fear of flying.
Reasons
- The national prescribing guidelines followed by GPs (the British National Formulary – BNF) states that all benzodiazepines are ‘contraindicated’ (not allowed) in treatment of phobias (fear conditions, such as fear of flying). It also states that the use of benzodiazepines to treat short-term anxiety is ‘inappropriate’. Benzodiazepines are only licensed for short-term use in a generalised anxiety crisis – but if this is the case for you, you should seek proper care and support for your mental health, and it would not be advisable to go on a flight. Your GP would be taking a significant legal risk by prescribing against these national guidelines.
- Diazepam is a sedative, so it makes you sleepier. If an emergency occurred during the flight, this could impair your ability to concentrate, follow instructions, or react to the situation. This could seriously affect the safety of you and the people around you. Such incidents are rare but they do occur, and it can be fatal if you are unable to evacuate the plane properly (an example event is flight BA28M, where 55 people sadly died while the plane burned while sat on Manchester Airport runway, and the official AAIB incident report specifically commented on evacuation delays contributing to the deaths). No-one else on board a plane will evacuate for you – the cabin crew are there to guide an evacuation, but you need to be responsible for yourself. As a result, many airlines consider sedative medications as a reason why someone would not be allowed on a plane, in a similar way that someone who has consumed excessive alcohol may be removed from a plane.
- Sedative drugs can make you fall asleep; however, the sleep is an unnatural non-REM sleep. Your movements during this type of sleep are reduced and this can place you at an even higher risk of developing blood clots in the legs (deep vein thrombosis – a DVT) or lungs (pulmonary embolism – a PE). These blood clots are very dangerous and can even be fatal. This risk further increases if your flight is over 4 hours long.
- Going on an aeroplane normally involves your blood oxygen levels decreasing from around 98% to as low as 90%, due to the air pressure decrease at cruising altitudes. Normally your body compensates for this by altering the rate and depth of your breathing. However, benzodiazepines work to depress your breathing and this can put you at risk of hypoxia (excessively low blood oxygen), especially if you have lung problems already, which can be very dangerous.
- Most people feel sleepy when they take diazepam, but a small proportion of people experience the opposite effect and can become aggressive. This is called a paradoxical effect, and it can be unexpectedly inconsistent, even if diazepam has been used in the past. Alongside aggression and agitation, this response can cause disinhibition and make you behave in ways you normally wouldn’t. This could also impact on your safety and the safety of your fellow passengers or could lead you to get in trouble with the law. Recently, a passenger in this situation was detained by the aircrew, arrested after an emergency landing, given jail time, and was also fined for the costs of redirecting the plane.
- In several countries, diazepam and similar drugs are illegal (Greece, Japan, and many Middle Eastern countries including the UAE are just some examples). They would be confiscated, and you might find yourself in trouble with the police for being in control of an illegal substance, even if it has been prescribed by a doctor in the UK. This has led to people spending time in a jail a foreign country.
- Diazepam has a long half-life, which means it stays in your system for a significant time. If your job requires you to submit random drug testing, you may fail these tests.
- There is a possible link between occasional use of benzodiazepines and earlier onset of dementia in later life.
What you can do
A fear of flying is frightening and can be debilitating. However, there are much better and effective ways of tackling the problem. We recommend you tackle your problem with a Fear of Flying Course, which are aviation-industry approved and are run by several airlines. These courses are far more effective than diazepam and have none of the undesirable effects. Also, the positive effects of the courses continue after the courses have been completed.
Easy Jet: www.fearlessflyer.easyjet.com
Tel: 0203 813 1644
British Airways:Flying with confidence | Information | British Airways
Tel: 01252 793 250
Virgin Atlantic: Welcome to Lovefly®
Tel: 01423 714 900
Ultimately, if you still feel unable to fly, then it may be appropriate to consider alternative routes of transport.
If you still wish to consider diazepam for fear of flying, we suggest consulting with a private GP or a private travel clinic, who may be able to help you further. These services are private and not offered by the NHS. The private clinics may then liaise with the airlines directly to arrange a medically-trained escort for a passenger who is taking sedative medications, which can be expensive.
Other situations – scans, dental appointments etc.
We do not routinely provide sedative medications such as diazepam for use in other situations, such as for dental/hospital procedures or scans.
The Royal College of Radiologists sets out clear guidance for sedation in hospital radiology departments (https://www.rcr.ac.uk/system/files/publication/field_publication_files/bfcr182_safe_sedation.pdf) which states “Sedation and analgesia should be administered by a competent and well-trained sedation and oversight provided by a sedation committee within the institution”.
The Intercollegiate Advisory Committee for Sedation in Dentistry has a similar guideline (https://www.saad.org.uk/IACSD%202020.pdf) which states “The monitoring and discharge requirements for oral sedation are the same as for intravenous sedation. Oral sedation must only be administered in the place where the dental treatment is provided and must only be carried out by practitioners who are already competent in intravenous sedation.”
As a result, responsibility for this type of treatment lies with your dentist or hospital staff, and not your GP.
Privacy Policy
As data controllers, GPs have fair processing responsibilities under the Data Protection Act and GDPR law 2018. This means ensuring that your personal confidential data (PCD) is handled in ways that are safe, transparent and what you would reasonably expect. Please find documents and links below.
- GDPR Privacy Policy last updated May 2023
- COVID19 Privacy Notice v6 August 2023 valid until end May 2024
- GDPR Children Privacy Notice last updated October 2021
- GDPR Employee Privacy Notice last updated October 2021
- GDPR Candidate Privacy Notice last updated October 2021
- Data Protection Policy
- Telephone recording policy
- Data Protection Act Fair Processing Patient Information Leaflet
- Your Data Matters to the NHS
The Practice Data Protection Officer is Paul Couldrey of PCIG Consulting Limited. Any queries regarding Data Protection issues should be addressed to him at paul.couldrey@nhs.net.
Paul Couldrey,
PCIG Consulting Limited
7 Westacre Drive,
Quarry Bank,
Dudley,
West Midlands,
DY5 2EE
Publication of earnings 2023-24
It is a contractual requirement for practices to publish their mean average earnings for 2023/24. Practices must;
- Publish details on their website by 31 March 2025.
- If asked this must also be available in paper copy or you can show the patient the information posted on the website.
The calculation excludes certain types of income and the rules are complex and open to interpretation.
Full time GP’s are defined in the guidance as working eight sessions or more. The number of GP’s includes salaried GP’s and locums who worked full or part time for 6 months or more.
All GP practices are required to declare the mean earnings for GPs working to deliver NHS services to patients at each practice.
The average pay for GPs working in Urmston Group Practice in the last financial year was £57,596 before tax and National Insurance. This is for 4 full time GPs and 7 part time GPs and 1 Locum GP who worked in the practice for more than six months.
Social Media Zero Tolerance Policy
Following activity on Social Media where patients of Urmston Group Practice have posted derogatory comments about the practice and some of our staff; we now have a Social Media Zero Tolerance Policy in place. If any such posts are brought to our attention, they could be viewed as a potential breakdown in the doctor-patient professional relationship and may result in the individual being removed from our list. We may contact the patients involved and invite them to have a discussion with the practice manager or one of the GP Partners to explore any issues they may have. We welcome all feedback as it gives us the opportunity to review the services that we provide and, where necessary or appropriate, make changes or improvements. We would ask that rather than posting derogatory or hurtful comments about the practice or any of our staff on social media, please speak to us about this or put your comments to us in writing giving us the opportunity to respond. Posting derogatory or offensive comments online can cause unwarranted distress to our practice members and staff. They may also cause other patients to delay or dissuade them from presenting to the surgery to receive medical treatment. Please consider the impact of your online activity before you post a comment.
Violence Policy
The NHS operate a zero tolerance policy with regard to violence and abuse and the practice has the right to remove violent patients from the list with immediate effect in order to safeguard practice staff, patients and other persons.
Violence in this context includes actual or threatened physical violence or verbal abuse which leads to fear for a person’s safety. In this situation we will notify the patient in writing of their removal from the list and record in the patient’s medical records the fact of the removal and the circumstances leading to it.